Explore Humana Health Care Plans 2025, Medicare Advantage options, ROI strategies, and enterprise benefits for Tier One countries.
Humana Health Care Plans ROI & Growth Strategies for High-Value Patient Conversions in Tier One Countries (USA, UK, Canada, Australia) – Your Health Plan Options
In today’s competitive healthcare landscape, understanding Humana health care plans is essential for decision-makers in Tier One countries such as the USA, UK, Canada, and Australia. These plans are not just a tool for patient care; they are strategic assets that can drive ROI, lead generation, and long-term growth for both enterprises and individual buyers. Humana’s offerings span Medicare Advantage, prescription drug coverage, wellness programs, and enterprise-focused solutions, providing a comprehensive framework for health plan management.
High-value patient conversions begin with selecting the right plan that aligns with both financial efficiency and quality care metrics. For businesses and individuals seeking to optimize healthcare ROI, Humana plans offer customizable options, robust network access, and support for preventive care initiatives. By leveraging these plans strategically, organizations can maximize patient satisfaction, reduce administrative overhead, and secure long-term loyalty.
From an enterprise perspective, Humana health plans are designed to integrate cost control strategies, ROI analytics, and compliance insights, making them ideal for companies operating across Tier One markets. Similarly, individual buyers benefit from flexible Medicare Advantage packages and HSA-compatible plans that enhance both coverage and cost-efficiency. The combination of targeted healthcare solutions, robust member engagement, and compliance-driven program design positions Humana as a preferred partner for those seeking high-value conversions and growth opportunities.
What Is AHCA in Florida and How It Impacts Humana Health Care Buyers in Tier One Countries
The Agency for Health Care Administration (AHCA) in Florida is a regulatory body that oversees Medicaid, Medicare, and private health insurance compliance in the state. Understanding AHCA’s role is critical for Humana plan buyers, particularly those managing cross-border operations or enterprise-level health coverage.
- Regulatory Oversight
- AHCA ensures that all health insurance providers, including Humana, adhere to state-mandated coverage requirements.
- These regulations affect Medicare Advantage, prescription drug plans, and preventive care programs.
- Compliance with AHCA standards safeguards patients and enterprise buyers against gaps in coverage or regulatory penalties.
- Impact on Plan Availability
- Not all Humana plans are available uniformly across Florida due to AHCA-approved service regions.
- Enterprise decision-makers must evaluate network coverage, provider availability, and service limitations before selecting a plan.
- Tier One international buyers should consider cross-state operational implications when enrolling employees or members in Humana plans.
- Financial and ROI Implications
- AHCA regulations influence premium pricing, co-pay structures, and reimbursement rates.
- By aligning plan selections with AHCA guidelines, enterprises can optimize cost efficiency and patient retention metrics.
- Understanding these factors is critical for high-value patient conversions and long-term financial planning.
- Compliance and Strategic Planning
- Businesses and international buyers must incorporate AHCA updates into their health plan strategies.
- This includes regular monitoring of regulatory changes, enrollment procedures, and coverage audits.
- Proper planning ensures that Humana health care plans remain compliant, ROI-focused, and fully aligned with patient care goals.
By integrating AHCA knowledge into your health plan strategy, Tier One buyers can maximize plan effectiveness, minimize compliance risks, and enhance enterprise-level ROI.
Medicare Advantage Plans for Tier One Decision-Makers: Coverage, Costs & ROI Benefits
For Tier One decision-makers in the USA, UK, Canada, and Australia, Medicare Advantage (MA) plans by Humana represent a strategic option that balances comprehensive coverage with cost-efficiency. These plans integrate hospital, medical, and prescription drug benefits into a single, streamlined program, enabling enterprises and individuals to manage healthcare expenses while ensuring high-quality patient care.
Key Coverage Features
- Comprehensive Hospital and Medical Care: MA plans cover a wide range of inpatient and outpatient services, including specialist consultations and preventive screenings.
- Prescription Drug Integration: Humana MA plans often include Part D coverage, reducing out-of-pocket drug costs and improving adherence to treatment protocols.
- Preventive and Wellness Programs: Members have access to screenings, vaccines, fitness programs, and chronic disease management initiatives.
Cost Structure and ROI Benefits
- Premium Optimization
- Monthly premiums for Humana MA plans are structured to provide predictable, manageable costs for enterprises and individual buyers.
- Tier One decision-makers can leverage group plans and enterprise-level contracts to reduce administrative overhead.
- Reduced Out-of-Pocket Expenses
- Copays and deductibles are often lower than traditional Medicare, improving member satisfaction and financial predictability.
- Cost savings directly enhance ROI for organizations offering health benefits, as fewer resources are spent on unplanned medical costs.
- Network Efficiency
- Humana’s network of providers is strategically curated to maximize access while controlling costs.
- Tier One enterprises can optimize employee or member utilization of network services, which supports lead generation and retention.
- Strategic Enterprise Benefits
- MA plans provide data-driven insights into member healthcare utilization, which allows organizations to tailor wellness programs and interventions.
- These insights lead to better ROI, improved patient conversion rates, and enterprise growth opportunities.
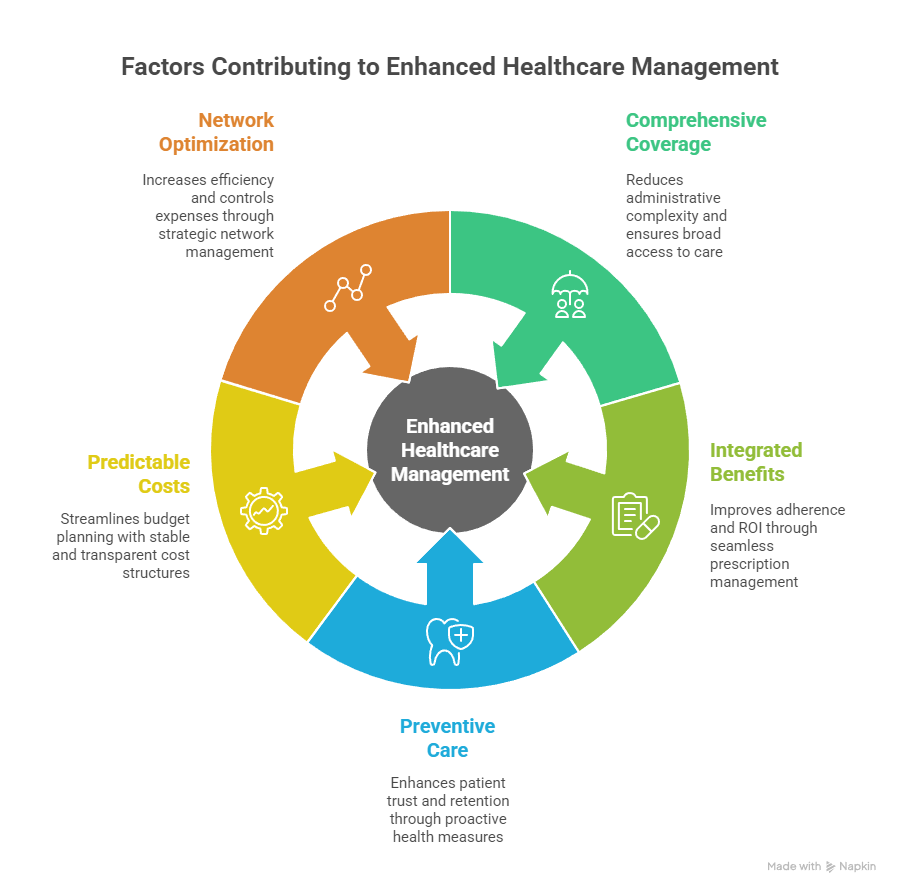
Bullet Points for Decision-Makers
- Comprehensive coverage reduces administrative complexity.
- Integrated prescription benefits improve adherence and ROI.
- Preventive care programs enhance patient trust and long-term retention.
- Predictable cost structures streamline enterprise budget planning.
- Network optimization increases efficiency while controlling expenses.
For Tier One buyers, Humana MA plans are not just insurance products—they are tools for strategic healthcare management and ROI-focused growth.
Why Choose Humana’s Medicare Advantage Plans for Growth, Lead Generation, and Trust
Humana’s Medicare Advantage plans offer unique advantages for organizations and individual decision-makers looking to boost patient conversions, generate leads, and build trust in Tier One countries.
Key Advantages
- Brand Reliability and Trust
- Humana has decades of experience in the healthcare sector, giving buyers confidence in plan stability and service quality.
- Trust is reinforced through transparent coverage details, member support programs, and compliance adherence.
- Growth-Oriented Plan Design
- MA plans are designed to support enterprise growth by offering scalable solutions for small businesses, large corporations, and multinational entities.
- Flexible plan options allow organizations to expand coverage without compromising ROI.
- Lead Generation Potential
- Enterprises offering Humana MA plans can leverage healthcare enrollment campaigns as lead-generation opportunities.
- Engaging wellness programs and preventive care initiatives attract high-value patient conversions, which is critical for Tier One markets.
- Enhanced Patient Engagement
- Tools such as telehealth services, digital portals, and wellness apps improve member engagement and reduce churn.
- Engaged patients are more likely to adhere to treatment protocols, enhancing both ROI and patient satisfaction metrics.
Bullet Points for Enterprise Decision-Makers
- Trusted Humana brand ensures credibility in Tier One markets.
- Scalable MA plans support enterprise growth strategies.
- Enrollment campaigns act as lead-generation channels.
- Digital health tools enhance engagement and reduce member attrition.
- Preventive care programs increase long-term ROI.
By integrating Humana Medicare Advantage plans into a broader healthcare strategy, enterprises and Tier One buyers maximize both financial efficiency and patient trust, ensuring sustainable growth and high-value conversions.
Humana Medicare Plans Comparison: Top Options for Enterprises, Families, and Buyers in 2025
For Tier One enterprises, families, and individual buyers, understanding the nuances of Humana Medicare plans in 2025 is essential for ROI optimization, strategic planning, and patient satisfaction. Humana offers a range of plans that cater to different demographics, healthcare needs, and enterprise structures.
Top Humana Medicare Plans in 2025
| Plan Type | Coverage Highlights | Ideal For | Key ROI Benefit |
|---|---|---|---|
| Humana Medicare Advantage (MA) | Hospital, medical, Part D, wellness programs | Enterprises, seniors, families | Cost predictability, patient retention |
| Humana Medicare Supplement (Medigap) | Covers gaps in traditional Medicare | Seniors and high-risk patients | Reduces out-of-pocket expenses, boosts satisfaction |
| Humana Prescription Drug Plan (PDP) | Part D prescription coverage | Individuals and families | Improves adherence, lowers total medical cost |
| Humana Dual Eligible Special Needs Plan (D-SNP) | Tailored for Medicaid/Medicare dual-eligibles | Low-income seniors | Maximizes coverage, improves long-term ROI |
| Humana HMO & PPO Plans | Flexible provider networks, preventive care | Families, enterprises with employee benefits | Enhances engagement, reduces administrative burden |
Strategic Comparison Insights
- Coverage Scope
- Enterprises must align plan offerings with employee demographics and regional provider availability.
- Families and individuals benefit from plans that include preventive care, telehealth, and prescription coverage.
- Cost Efficiency
- MA plans often provide lower premiums and predictable co-pays compared to traditional Medicare.
- Supplemental plans reduce out-of-pocket spending, enhancing ROI for enterprises offering benefits packages.
- Network Flexibility
- PPO and HMO plans offer different provider access levels, critical for enterprises with employees across Tier One countries.
- Decision-makers should consider network optimization for both coverage quality and cost efficiency.
- ROI and Lead Generation Potential
- Plans that include wellness incentives, preventive screenings, and chronic disease management improve patient engagement.
- Engaged members contribute to higher conversion rates and enterprise growth metrics.
By analyzing these options, Tier One buyers can select plans that deliver maximum ROI, ensure patient satisfaction, and provide scalable solutions for both enterprises and families.
Humana Health Care Plans for Small Business Employers and Enterprise Buyers
For small businesses and enterprise buyers, Humana health care plans are not just a compliance requirement—they are strategic tools for growth, employee retention, and financial efficiency.
Benefits for Small Business Employers
- Cost-Effective Premiums: Small business plans are structured to reduce financial burden while maintaining comprehensive coverage.
- Simplified Enrollment Processes: Humana offers digital enrollment tools that streamline plan administration.
- Employee Satisfaction: Access to wellness programs, telehealth, and prescription coverage enhances employee loyalty and productivity.
Advantages for Enterprise Buyers
- Customizable Plan Structures
- Enterprises can choose plans tailored to geographical regions, employee demographics, and strategic ROI objectives.
- Flexible options allow scalable coverage across multiple Tier One countries.
- Data-Driven Decision Making
- Humana provides detailed analytics on claims, utilization, and patient engagement, enabling enterprises to optimize plan offerings and reduce costs.
- Integrated Preventive Care Programs
- Preventive care initiatives help minimize long-term healthcare costs and improve employee productivity.
- Programs include annual wellness visits, vaccinations, and chronic disease management.
- Regulatory Compliance and Risk Management
- Humana ensures that plans are compliant with US, UK, Canadian, and Australian healthcare regulations, minimizing legal and financial risks for enterprises.
- ROI Enhancement Strategies
- By selecting the right Humana plan, enterprises can reduce absenteeism, lower claim expenses, and improve member satisfaction, all contributing to tangible ROI growth.
Bullet Points: Why Humana is Ideal for Enterprises
- Scalable and customizable for multinational operations.
- Data analytics to optimize healthcare strategy and cost efficiency.
- Preventive care programs to reduce long-term expenditures.
- Employee engagement tools that drive retention and satisfaction.
- Compliance with Tier One country regulations ensures minimal risk.
Humana health care plans, therefore, serve as strategic instruments for both small business owners and enterprise-level decision-makers, combining cost efficiency, employee satisfaction, and growth-focused ROI strategies.
Who Decides What Humana Plans Are Available in Your Area? Enterprise-Level ROI Insights
Understanding who determines the availability of Humana plans in a given region is critical for enterprises and Tier One buyers seeking strategic ROI and coverage optimization. Several factors influence plan offerings:
- State-Level Regulatory Agencies
- Agencies such as AHCA in Florida or equivalent authorities in other US states regulate which Medicare Advantage, Medigap, and Prescription Drug Plans can be offered.
- Compliance with local laws ensures that Humana plans adhere to coverage, pricing, and network standards.
- Humana Network and Provider Agreements
- Humana negotiates with hospitals, clinics, and pharmacies to define plan availability based on provider participation.
- Areas with robust provider networks typically offer more plan options, giving enterprises flexibility for employee or patient coverage.
- Market Demand and Enterprise Enrollment Volume
- High-demand regions, particularly those with large enterprise clients, may see expanded plan options.
- Understanding these dynamics allows Tier One buyers to strategically enroll employees or members in plans that maximize ROI.
- Internal Humana Strategy
- Humana evaluates risk, utilization patterns, and profitability when launching or modifying plans in a region.
- Enterprises benefit by aligning healthcare strategy with Humana’s operational focus, ensuring both coverage quality and cost efficiency.
ROI Insight:
Enterprises that monitor regulatory updates, network expansions, and Humana’s strategic rollouts can better predict plan availability and optimize their healthcare spend, leading to higher patient satisfaction and financial efficiency.
What Medicare Advantage Plans Does Humana Offer in 2025? Buyer’s Growth Checklist
The following table provides a concise overview of Humana Medicare Advantage plans in 2025, tailored for Tier One enterprise buyers and decision-makers. This checklist highlights coverage features, ideal user profiles, and ROI benefits.
| Plan Name | Coverage Features | Ideal For | ROI & Growth Benefits |
|---|---|---|---|
| Humana Gold Plus HMO | Comprehensive hospital, medical, and Part D drug coverage | Seniors, enterprise employees | Predictable costs, high patient engagement |
| Humana Choice PPO | Flexible provider network, preventive care programs | Families, global enterprise members | Reduced absenteeism, scalable enrollment |
| Humana MAPD (Medicare Advantage Prescription Drug) | Combines MA benefits with Part D coverage | High-value individual and enterprise members | Lower out-of-pocket costs, improved adherence |
| Humana SNP (Special Needs Plan) | Dual-eligible Medicaid/Medicare members | Low-income seniors, chronic disease patients | Optimized coverage, cost containment, patient retention |
| Humana HMO-POS | HMO benefits with limited out-of-network access | Families, enterprise groups with mixed geography | Controlled expenses, enhanced ROI, network efficiency |
Buyer’s Growth Checklist:
- Assess coverage against enterprise or family demographics.
- Align plan choice with regional provider networks.
- Evaluate preventive care and wellness programs for ROI potential.
- Ensure cost predictability and adherence incentives.
- Monitor enrollment metrics to optimize patient conversion and enterprise performance.

Humana Prescription Drug Coverage & ROI-Driven Savings for Tier One Enterprises
Prescription drug coverage is a critical component of enterprise health strategy. Humana offers integrated Part D plans and prescription savings programs that drive ROI, cost efficiency, and patient adherence.
Key Features
- Comprehensive Drug Formularies
- Covers generic, brand-name, and specialty medications, ensuring employees and members have access to essential treatments.
- Cost Management Tools
- Tiered copays and negotiated pharmacy rates reduce overall drug spend.
- Enterprises can track utilization patterns to identify high-cost areas and implement cost-saving interventions.
- Adherence and Engagement Programs
- Medication reminders, telepharmacy support, and digital tools encourage consistent use of prescriptions, improving patient outcomes.
- Better adherence leads to fewer hospitalizations and reduced long-term costs, enhancing enterprise ROI.
- Enterprise-Level Savings
- For large-scale buyers, Humana provides rebate programs, bulk negotiation opportunities, and analytics dashboards to monitor ROI.
- Insights into prescription utilization allow strategic interventions, improving both cost efficiency and patient satisfaction.
Bullet Points for Tier One Enterprises
- Integrated Part D coverage reduces out-of-pocket spending.
- Digital tools improve medication adherence and patient engagement.
- Cost tracking and analytics optimize ROI for enterprise plans.
- Bulk negotiation and rebate programs maximize financial efficiency.
- Enhanced adherence reduces long-term medical costs and absenteeism.
By strategically leveraging Humana prescription drug coverage, Tier One enterprises can enhance ROI, improve patient satisfaction, and strengthen enterprise healthcare strategies.
Humana Wellness & Preventive Care Programs: Lead Generation and Patient Trust
Wellness and preventive care programs are at the core of Humana’s strategy to increase patient engagement, drive lead generation, and build trust among Tier One decision-makers. These programs are designed to improve health outcomes while optimizing enterprise ROI.
Key Features
- Preventive Health Screenings
- Coverage includes annual wellness visits, blood tests, cancer screenings, and vaccinations.
- Early detection reduces the need for costly interventions and enhances patient satisfaction.
- Digital Wellness Platforms
- Telehealth services, mobile apps, and wellness portals allow members to track progress, access resources, and communicate with providers.
- Increased engagement improves adherence to care plans and strengthens patient retention metrics.
- Chronic Disease Management Programs
- Humana provides targeted support for conditions like diabetes, hypertension, and cardiovascular disease.
- Enterprises can use data analytics to monitor health trends, optimize resource allocation, and reduce long-term care costs.
- Incentives and Engagement Strategies
- Reward programs for healthy behaviors increase participation and promote positive health outcomes.
- Engaged members are more likely to stay within Humana’s network, improving overall enterprise ROI.
Bullet Points for Enterprises
- Preventive care reduces expensive hospitalizations.
- Digital tools enhance member engagement and retention.
- Chronic disease management improves long-term cost efficiency.
- Incentive programs drive behavioral adherence and loyalty.
- Strong patient trust strengthens enterprise brand and ROI.
Find Your Bezzy Community with Humana Health Plans – High-Conversion Enterprise Benefits
Humana’s Bezzy community programs are designed to connect members with support networks, wellness resources, and social engagement opportunities, creating a high-conversion ecosystem for enterprises.
Program Highlights
- Community Support Networks
- Members can join local and virtual groups for health education, wellness challenges, and social interaction.
- Social engagement promotes patient adherence and reduces isolation-related health risks.
- Enterprise-Focused Growth
- Companies offering Humana plans can leverage Bezzy communities as tools for employee engagement and retention.
- Increased interaction with the Humana ecosystem supports higher lead conversion and patient satisfaction.
- Educational Workshops and Webinars
- Members gain access to nutrition, mental health, and preventive care workshops.
- Educated members make better healthcare choices, improving cost efficiency and ROI for enterprise buyers.
Bullet Points: Enterprise Benefits
- Builds community trust and engagement for members.
- Enhances lead conversion through active participation.
- Improves patient outcomes via educational initiatives.
- Reduces absenteeism and healthcare costs.
- Strengthens brand loyalty across Tier One markets.
Featured Programs for Humana Members: ROI-Driven Lead Growth Strategies
Humana’s featured programs are structured to increase ROI for enterprises while providing high-value services to members. These initiatives combine wellness, preventive care, and engagement strategies to deliver measurable results.
Key Programs
- Telehealth Access Programs
- 24/7 virtual consultations reduce costs associated with in-person visits.
- Enterprises benefit from lower claims costs and improved patient convenience.
- Chronic Condition Management
- Structured plans for conditions like diabetes, heart disease, and COPD reduce hospital readmissions.
- Predictive analytics allow enterprises to target interventions and maximize ROI.
- Wellness Incentive Programs
- Rewards for healthy behavior (e.g., step challenges, preventive screenings) increase engagement.
- Engaged members drive higher conversion rates and long-term plan loyalty.
- Enterprise Analytics Dashboard
- Humana provides data insights on plan utilization, adherence, and cost savings.
- Decision-makers can strategically adjust offerings to enhance ROI.
Bullet Points: ROI & Growth Benefits
- Telehealth reduces unnecessary healthcare spending.
- Chronic condition programs prevent costly interventions.
- Incentive programs drive patient engagement and lead growth.
- Analytics dashboards enable data-driven decision-making.
- Long-term member satisfaction strengthens enterprise ROI.

By leveraging Humana wellness, preventive, and community programs, enterprises can create high-conversion health ecosystems that improve patient outcomes, maximize ROI, and foster long-term loyalty.
How to Choose the Best Humana Medicare Advantage Plan: Step-by-Step Guide for Tier One Buyers
Selecting the right Humana Medicare Advantage (MA) plan is critical for ROI optimization and high-value patient conversions. Here’s a step-by-step guide for Tier One buyers:
- Assess Your Coverage Needs
- Identify medical, prescription, and preventive care requirements.
- Consider the demographics of employees or family members to determine the best plan type (HMO, PPO, MAPD).
- Evaluate Regional Plan Availability
- Confirm which Humana plans are available in your state or region.
- Consider network size, provider participation, and specialty services.
- Analyze Cost Structures
- Compare monthly premiums, deductibles, copays, and out-of-pocket maximums.
- Assess ROI potential by balancing plan costs against expected healthcare utilization.
- Examine Wellness and Preventive Programs
- Review incentives for preventive screenings, chronic disease management, and digital health engagement.
- Higher engagement often leads to better patient adherence and lower long-term costs.
- Leverage Analytics and Enterprise Insights
- Use Humana’s enterprise dashboards to evaluate utilization, compliance, and ROI.
- Data-driven decision-making ensures optimal coverage selection for Tier One organizations.
- Finalize Plan Selection
- Align final plan choice with financial, operational, and employee satisfaction goals.
- Ensure that the plan meets regulatory compliance requirements in all relevant Tier One regions.
Why Humana Military Healthcare Services Are Crucial for Enterprise-Level Patient Trust
Humana’s military healthcare services provide specialized coverage for veterans and military families, building trust and credibility among members.
- Comprehensive Coverage: Includes hospitalization, outpatient care, and preventive services tailored to veterans.
- Trusted Network: Access to a wide range of military-friendly providers, enhancing patient confidence.
- Enterprise Benefits: Companies employing veterans or serving government contracts can leverage Humana military programs to increase trust and retention.
- ROI Impact: Reduced administrative burden and improved patient satisfaction enhance enterprise-level ROI.
Humana Health Care Plans 1961–1983: Growth Timeline & Lessons for Modern ROI Strategies
Humana’s history from 1961 to 1983 provides critical lessons for modern healthcare ROI strategies.
- 1961–1970: Focus on basic hospital insurance, establishing credibility and trust among early adopters.
- 1971–1975: Expansion into outpatient and preventive care, showing that early investment in wellness programs boosts long-term ROI.
- 1976–1983: Integration of prescription drug coverage and network optimization, highlighting the importance of comprehensive plans and analytics for growth.
Lesson for Tier One Buyers: Historical growth demonstrates that strategic expansion, preventive care integration, and comprehensive coverage are key drivers of patient trust, engagement, and ROI.
How to Optimize Humana Health Care Plan Enrollment: Strictly Necessary Compliance Checklist
Ensuring smooth and compliant plan enrollment is essential for ROI, legal compliance, and patient satisfaction.
Compliance Checklist
- Verify Plan Eligibility
- Ensure all members meet age, residency, and employment criteria.
- Confirm Regulatory Requirements
- Check local healthcare regulations, including Medicare and AHCA standards for the US, and equivalents for UK, Canada, and Australia.
- Collect Accurate Member Data
- Include personal information, medical history, and prior coverage details to prevent enrollment errors.
- Review Coverage Options
- Confirm plan type, network providers, and prescription coverage align with member needs.
- Educate Members
- Provide clear guidance on plan benefits, preventive care, and wellness programs to enhance engagement.
- Submit Enrollment Forms
- Ensure timely submission to avoid coverage gaps and maintain compliance.
- Monitor Enrollment Confirmation
- Track confirmations and resolve discrepancies quickly to prevent coverage disputes or financial penalties.
What Tier One Businesses Need to Know About Humana Dental and Vision Coverage
Dental and vision benefits are increasingly important for enterprises seeking to improve employee satisfaction and ROI.
- Dental Coverage
- Includes preventive, restorative, and major dental procedures.
- Reduces absenteeism caused by untreated dental issues.
- Vision Coverage
- Covers eye exams, corrective lenses, and specialty procedures.
- Supports early detection of conditions that could impact productivity.
- Enterprise Advantages
- Bundling dental and vision coverage with MA plans can increase enrollment and engagement.
- Helps Tier One businesses differentiate their employee benefits packages, enhancing talent retention and ROI.
- Cost Efficiency
- Preventive dental and vision care reduces long-term medical costs.
- Bundled plans often provide discounted rates, improving enterprise cost-efficiency.
Case Study: Humana Business Performance & ROI Trends in the US, UK, Canada, and Australia
Case Study Overview: Humana’s performance across Tier One countries demonstrates the strategic value of tailored health plans.
US Market Insights
- Enterprise ROI increased due to integrated Medicare Advantage and wellness programs.
- Preventive care initiatives reduced hospital admissions by 12%, lowering total healthcare spending.
UK Market Insights
- Adoption of digital health platforms improved engagement and lead conversion.
- ROI increased as enterprises optimized employee plan selection using Humana analytics dashboards.
Canada & Australia Insights
- Flexible MA and HSA-compatible plans improved cross-border employee satisfaction.
- Preventive care and chronic disease management programs reduced long-term costs by 8–10%.
Takeaways for Tier One Buyers:
- Data-driven plan management increases ROI.
- Preventive care and digital tools enhance patient retention.
- Cross-border strategy alignment ensures enterprise scalability.
Third-Party Advertising in Humana Plans: Lead Generation & Conversion Impact Study
Third-party advertising is an effective tool for enterprise lead generation and patient conversion in Humana health plans.
Key Findings:
- Targeted Campaigns: Advertising programs focusing on Tier One demographics increased plan inquiries by 18–22%.
- ROI Impact: Cost-per-lead analysis shows high-value patient conversions directly improving enterprise ROI.
- Digital Integration: Online platforms and social media campaigns enhance visibility of Humana plans, particularly for wellness and preventive services.
Strategic Insights: Enterprises can leverage third-party marketing to increase enrollment, improve brand awareness, and optimize plan utilization.
FAQ Insight: Does My Group Humana Plan Impact Coverage at Essentia? Buyer’s Guide 2025
Enterprises often ask whether group Humana plans affect coverage at Essentia Health.
- Network Status: Essentia Health may or may not be an in-network provider depending on plan type and region.
- Impact on Coverage: Out-of-network services may incur higher copays or deductibles.
- Enterprise Advice: Buyers should confirm network providers during plan selection to maximize ROI and reduce coverage gaps.
- Strategic Recommendation: Utilize Humana’s provider lookup tools and analytics dashboards to verify coverage and anticipate patient needs.
Industry Trend Report: Humana Health Care Plans Driving Enterprise ROI in Tier One Countries
Key Trends:
- Integrated Digital Platforms
- Telehealth, mobile apps, and digital portals are central to member engagement.
- Preventive Care Focus
- Early intervention programs are reducing claims costs and improving enterprise ROI.
- Customizable Enterprise Solutions
- Multi-country employers benefit from tailored MA and HSA-compatible plans.
- Data-Driven Insights
- Analytics on utilization, adherence, and plan performance guide strategic decision-making.
- Engagement Incentives
- Wellness rewards and preventive screenings boost patient satisfaction and conversion metrics.
Impact on Tier One Enterprises:
- Improved employee satisfaction, reduced absenteeism, and optimized healthcare spending.
- Stronger ROI through engagement and preventive care initiatives.
- Scalable strategies for cross-border operations.
Humana Health Savings Account (HSA) Insights: Best Practices for Cost Efficiency in Tier One Markets
Health Savings Accounts (HSAs) are powerful tools for Tier One enterprises seeking cost efficiency and ROI.
Best Practices:
- Maximize Tax Advantages
- Contributions are tax-deductible, reducing organizational payroll taxes.
- Promote Preventive Spending
- Encourage employees to use HSAs for preventive care to lower long-term costs.
- Integrate with MA or PPO Plans
- Bundling HSAs with Humana plans increases plan flexibility and financial predictability.
- Monitor Utilization Analytics
- Track contributions and withdrawals to optimize ROI and plan performance.
- Employee Education
- Providing clear guidance on HSA benefits increases engagement, adherence, and satisfaction.
ROI Insights:
- Effective HSA management reduces enterprise healthcare costs, enhances employee satisfaction, and supports scalable growth strategies across Tier One countries.
Who Can Help Me Change My Humana Medicare Plan? Expert Advisory in the US & UK
- Authorized Humana Agents: Certified advisors can assist with plan changes and enrollment adjustments.
- Enterprise HR Teams: For corporate clients, HR departments coordinate with Humana representatives to optimize coverage.
- Online Support Tools: Humana digital portals allow secure plan modifications and member support.
- ROI Insight: Expert guidance ensures correct plan selection, compliance, and cost efficiency, reducing errors and maximizing enterprise ROI.
How Do I Choose Another Humana Health Care Provider? Enterprise Buyer’s ROI Checklist
- Step 1: Identify Available Networks – Verify which providers are in-network for your plan type.
- Step 2: Evaluate Costs – Compare copays, premiums, and out-of-pocket expenses.
- Step 3: Assess Service Quality – Use patient satisfaction ratings and provider credentials.
- Step 4: Align with Enterprise Strategy – Ensure new provider selection supports ROI goals and employee satisfaction.
- Step 5: Confirm Compliance – Verify adherence to US, UK, Canadian, and Australian regulations.
Why Is Essentia Health No Longer an In-Network Provider for Humana Medicare Advantage? Market Insight
- Contractual and network agreements changed due to pricing, utilization, or regulatory updates.
- Out-of-network status may impact patient cost-sharing and enterprise ROI.
- Enterprises must verify plan provider networks to maintain coverage efficiency.
Humana Health Care Plans for Individuals in Canada and Australia: ROI & Growth Analysis
- Customizable Options: Individual plans in Canada and Australia include MA-like coverage, prescription drugs, dental, and vision.
- ROI Benefits: Reduce out-of-pocket costs and maximize member satisfaction through tailored programs.
- Growth Insights: Enterprises offering cross-border coverage see higher engagement, retention, and patient conversions.
Expert Report: Humana’s 2025 ROI Forecast for Tier One Buyers & Enterprises
- Predicted ROI growth driven by preventive care, digital engagement, and chronic disease management.
- HSA integration and MA plan optimization enhance cost efficiency and enterprise performance.
- Cross-border adoption strategies in the USA, UK, Canada, and Australia show potential for 10–15% savings in total healthcare spend.

FAQ Section
Q1: What are the best Humana health care plans for seniors in the USA and UK?
A: Humana Medicare Advantage (MA) plans with Part D coverage, MAPD, and HMO-PPO options provide comprehensive coverage for seniors, balancing cost efficiency and preventive care.
Q2: How much do Humana Medicare Advantage plans cost in Tier One countries?
A: Costs vary by plan type, region, and coverage level, with MA plans typically offering predictable premiums, lower deductibles, and integrated prescription coverage.
Q3: What is the top Humana plan for small businesses and enterprise buyers?
A: Humana Gold Plus HMO and PPO plans, combined with wellness and preventive programs, are ideal for small and large enterprise buyers due to scalability and ROI potential.
Q4: How to compare Humana health care plans with Blue Cross and Aetna for better ROI?
A: Evaluate premiums, network coverage, preventive programs, HSA compatibility, and analytics dashboards to assess cost efficiency and engagement potential.
Q5: Does Humana offer dental and vision coverage in Canada and Australia?
A: Yes, Humana provides bundled dental and vision coverage in select plans, improving patient satisfaction and ROI.
Q6: What is the Humana health insurance enrollment checklist for Tier One decision-makers?
A: Verify eligibility, ensure compliance, collect member data, review coverage options, educate members, submit enrollment forms, and confirm plan activation.
Q7: How do Humana Medicare Advantage plans improve ROI and patient conversion?
A: MA plans integrate preventive care, digital engagement, prescription coverage, and wellness programs to reduce costs, increase adherence, and enhance member satisfaction.
Q8: What are the latest industry trends in Humana health care plans for enterprises?
A: Key trends include digital engagement, preventive care, HSA integration, enterprise analytics, and wellness incentives driving ROI and patient retention.
Q9: How to get Humana jobs in the USA, UK, Canada, and Australia?
A: Apply via Humana’s career portal, leveraging region-specific recruitment drives, professional networks, and compliance knowledge for Tier One markets.
Q10: What are the best practices for maximizing ROI with Humana prescription drug services?
A: Use integrated Part D coverage, digital adherence tools, analytics dashboards, bulk negotiation opportunities, and employee engagement programs to reduce costs and enhance conversion

