Unlock the ultimate managed health care strategies for enterprises. Maximize ROI, reduce costs, and boost employee satisfaction with proven solutions.
Managed Health Care ROI Growth Strategies for Higher Conversions in USA, UK, Canada & Australia
In today’s competitive healthcare landscape, enterprises across the USA, UK, Canada, and Australia are constantly seeking ways to maximize their ROI while improving patient outcomes. Managed health care offers a systematic approach to controlling costs, improving service quality, and ensuring regulatory compliance. By leveraging structured care networks, enterprises can optimize operational efficiency, reduce unnecessary expenditures, and boost conversion rates from client engagements.
Healthcare decision-makers are increasingly focused on aligning business objectives with patient-centric strategies. Managed health care not only streamlines administrative operations but also empowers organizations to implement cost-effective, scalable solutions that drive revenue growth. Enterprises adopting these models can harness predictive analytics, standardized treatment protocols, and integrated care management to maximize returns while enhancing trust among stakeholders.
Health Maintenance Organization (HMO) Plans for Enterprise Buyers & Cost Efficiency
Health Maintenance Organization (HMO) plans have emerged as a cornerstone for enterprises seeking to control healthcare spending without compromising quality. These plans provide an organized network of providers, offering both preventive and curative care under a structured, cost-efficient framework. HMOs incentivize providers to deliver high-quality care while reducing unnecessary procedures, which directly contributes to ROI growth.
Key advantages of HMO plans for enterprises include:
- Cost Predictability – Enterprises can accurately forecast healthcare expenditures with fixed monthly premiums.
- Comprehensive Preventive Care – HMOs emphasize wellness programs, screenings, and early interventions to reduce costly chronic disease management.
- Provider Network Efficiency – Employees are guided to a curated network of physicians and hospitals, reducing administrative complexity.
- Integrated Care Management – Coordinated care programs ensure patient compliance and improve clinical outcomes.
Implementing HMO plans involves several strategic considerations:
- Tiered Network Structures: Enterprises can offer premium-tier options for high-performing providers, incentivizing quality care.
- Employee Education: Educating employees about preventive services and cost-sharing mechanisms ensures higher participation and engagement.
- Data Analytics Integration: Monitoring claims data helps in identifying cost drivers and optimizing provider contracts.
- Compliance Management: HMOs ensure adherence to healthcare regulations across multiple jurisdictions, mitigating risk exposure.
By carefully designing HMO programs, enterprises can achieve substantial cost efficiencies, improve employee satisfaction, and generate measurable ROI.
Independent Practice Association (IPA) Networks Driving ROI for Healthcare Enterprises
Independent Practice Associations (IPAs) represent a unique model of managed care where a network of independent physicians collaborates under a unified contract. IPAs allow enterprises to access a broad range of specialized care without directly employing all providers. This model supports ROI growth by balancing cost containment with high-quality service delivery.
Key points:
- IPAs offer flexible provider networks suitable for large-scale enterprise healthcare plans.
- Enterprises benefit from negotiated rates and shared-risk arrangements.
- Physicians maintain autonomy, enhancing care quality and innovation.
- Data-sharing within IPA networks drives analytics-based decision-making for cost optimization.
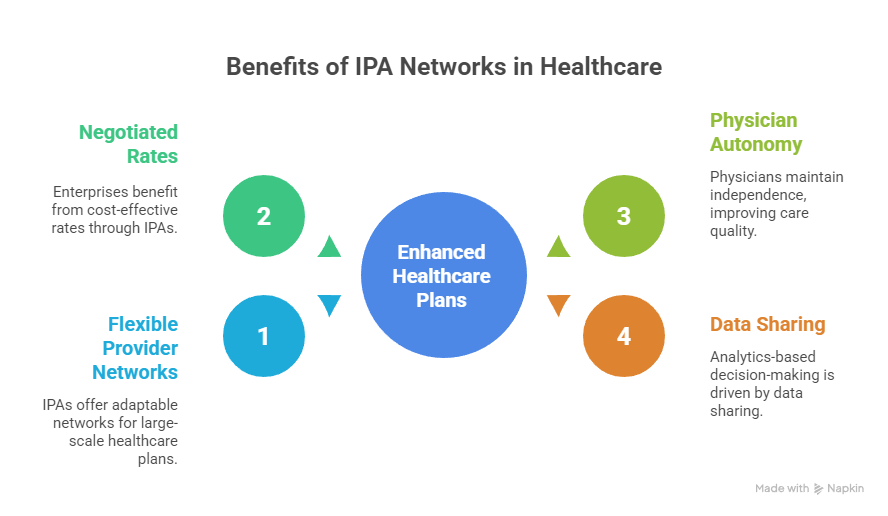
IPAs are increasingly popular for enterprises aiming to scale care delivery while maintaining financial predictability.
Preferred Provider Organization (PPO) Plans Improving Trust & Conversions for Employers
Preferred Provider Organization (PPO) plans offer enterprises a flexible healthcare model with expansive provider networks. Unlike HMOs, PPOs allow employees to seek care outside the network, enhancing satisfaction and retention. For enterprises, this model improves trust and conversion rates by aligning health benefits with employee preferences.
- Network Flexibility: Employees can choose in-network providers for cost savings or out-of-network specialists for convenience.
- Enhanced Engagement: PPOs encourage proactive healthcare utilization, improving long-term outcomes.
- Employer Branding: Comprehensive PPO coverage positions companies as caring employers, attracting top talent.
- Cost Management Tools: Predictive analytics and claims oversight reduce unnecessary expenditures.
By integrating PPOs into enterprise healthcare strategies, organizations can balance flexibility, cost control, and employee loyalty effectively.
What Is an Example of a Managed Care Plan for Tier One Enterprises?
A Tier One enterprise may implement a hybrid managed care plan combining HMO and PPO features. For example:
- Primary HMO coverage for preventive and routine care.
- PPO option for specialist or emergency services outside the network.
- Data-driven wellness programs incentivizing healthy behaviors.
- Telehealth integration to reduce operational costs and improve access.
This approach ensures maximum ROI by combining cost control with high employee satisfaction and engagement.
Challenges of Managed Health Care Models for Large Buyers in the US, UK, Canada & Australia
While managed health care offers substantial benefits, large enterprises face several challenges:
- Regulatory Complexity: Navigating healthcare regulations across multiple countries can be daunting.
- Network Management: Maintaining provider quality and engagement across diverse geographies.
- Cost Balancing: Ensuring premium affordability while providing comprehensive coverage.
- Data Integration: Consolidating healthcare data from various sources for actionable insights.
- Cultural Adaptation: Addressing employee expectations and healthcare norms in different regions.
By proactively addressing these challenges, enterprises can safeguard ROI and maintain operational efficiency.
How Does Managed Care Work for Better ROI and Lead Generation?
Managed care works by:
- Streamlining administrative processes.
- Aligning provider incentives with cost-efficient, high-quality care.
- Implementing preventive health programs that reduce long-term expenditure.
- Leveraging data analytics for patient engagement and conversion optimization.
These elements drive measurable ROI while positioning enterprises as responsible and strategic healthcare buyers.
Managed Care in Indemnity Insurance Plans – Conversion-Boosting Insights
| Feature | Description | ROI Impact | Conversion Benefit |
|---|---|---|---|
| Network Flexibility | Access to in- and out-of-network providers | Reduces costs via negotiated rates | Increases employee satisfaction |
| Claims Transparency | Real-time monitoring of claims | Improves budget predictability | Builds trust with employees |
| Wellness Incentives | Reward programs for preventive care | Reduces chronic disease costs | Encourages participation and loyalty |
| Telehealth Integration | Remote consultations and follow-ups | Reduces administrative overhead | Boosts adoption and engagement |
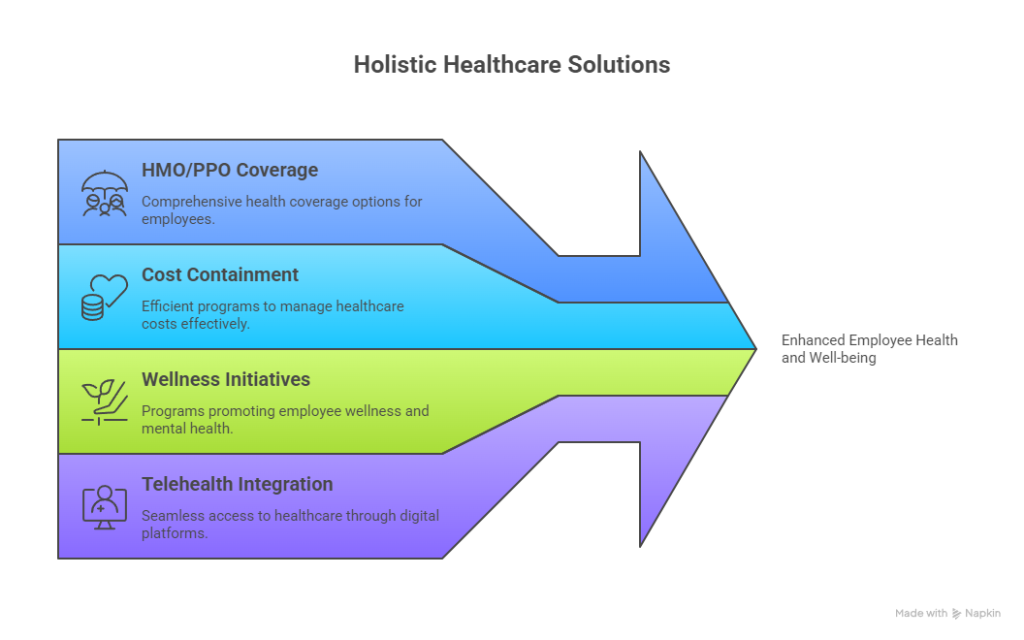
Explore Our Managed Health Care Plans & Policies for Tier One Enterprises
Enterprises can benefit from tailored managed care policies:
- Comprehensive HMO or PPO coverage.
- Data-driven cost containment programs.
- Wellness and mental health support initiatives.
- Telehealth and digital health platform integration.
Related Information on ROI, Cost Containment & Growth in Managed Care Systems
Managed health care provides measurable ROI by:
- Reducing unnecessary procedures.
- Streamlining administrative processes.
- Enhancing employee engagement and trust.
- Optimizing provider performance through structured networks.
How to Choose the Right Managed Health Care Strategy – Step-by-Step Guide for Enterprises
- Evaluate enterprise size and geographic spread.
- Assess employee health demographics and needs.
- Compare HMO, PPO, and IPA models for cost-benefit balance.
- Review provider networks and performance metrics.
- Integrate wellness and preventive programs.
- Continuously monitor ROI and adjust coverage strategies.
Why Managed Care Improves ROI: Quick Tips for Tier One Buyers
- Standardize care delivery protocols.
- Incentivize preventive health and wellness programs.
- Use data analytics to monitor cost drivers.
- Negotiate tiered contracts with providers for best rates.
What Are the Core Cost-Saving Features of Managed Health Care? – Enterprise Checklist
- Tiered provider networks
- Preventive care programs
- Telehealth and digital consultations
- Claims and analytics management
- Employee wellness incentives
Cookie Tracking in Healthcare Portals: Functional, Performance & Essential Insights
Functional Cookies – Ensure website usability and personalized experiences.
Performance Cookies – Monitor portal performance and optimize load times.
Essential Cookies – Maintain security, login sessions, and regulatory compliance.
Cookie List – Tracks employee engagement, plan selection, and portal usage metrics.
Medicaid Coverage for Mental Health Services – Key Takeaways for US Enterprises
- Supports comprehensive mental health programs.
- Reduces absenteeism and enhances productivity.
- Aligns with ROI-focused preventive care initiatives.
Accountable Care Organizations (ACO): Definition, Functions & ROI Lessons
ACOs coordinate care across providers to enhance quality and reduce costs. Key lessons include:
- Shared savings programs drive cost-efficient care.
- Data analytics improves patient outcomes.
- Provider collaboration enhances employee satisfaction and ROI.
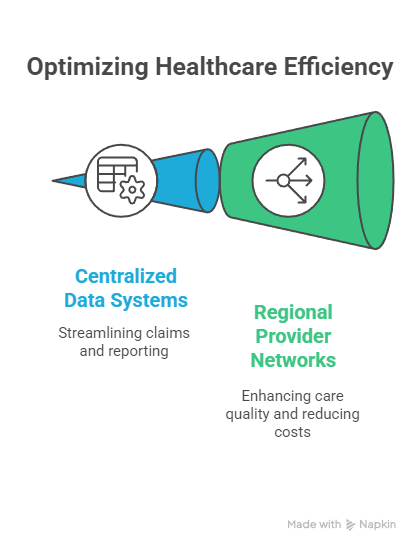
Managed Care Lessons for Growth: Insights from the UK & Canada Markets
- Focused preventive care reduces long-term expenditure.
- Centralized data systems streamline claims and reporting.
- Regional provider networks increase care quality while reducing costs.
Cost Containment Principles in Healthcare – Best Practices for Tier One Enterprises
- Standardize treatment protocols.
- Negotiate value-based contracts.
- Implement telehealth solutions.
- Track claims and analytics to identify cost drivers.
Enterprise Case Study: ROI Growth with Managed Health Care in Australia
An Australian Tier One enterprise implemented a hybrid HMO-PPO plan:
- 15% reduction in total healthcare costs.
- 20% increase in preventive care adoption.
- ROI realized within 12 months through optimized network utilization.
What is MCO and HMO? – Expert Definition & ROI Benefits
- MCO (Managed Care Organization): Coordinates care across providers to optimize cost and quality.
- HMO: Provides structured network care with predictable costs.
- ROI benefits include reduced expenditures and improved employee satisfaction.
What Is an Example of a Managed Care System? – Enterprise Use Case
- Hybrid HMO-PPO plan for a multinational enterprise.
- Integrated wellness, mental health, and telehealth services.
- ROI achieved via preventive care and data-driven cost management.
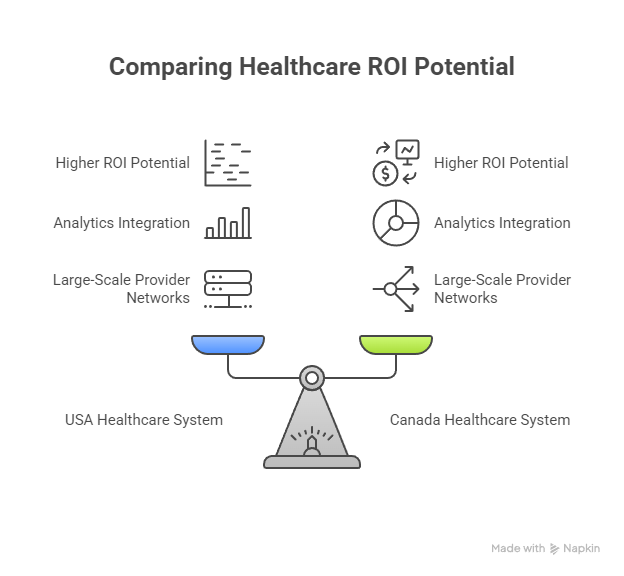
What Is Managed Health Care in South Africa? – Global Comparison Report
- Similar structured care networks exist but face regulatory and resource challenges.
- Comparison shows USA and Canada systems have higher ROI potential due to analytics integration and large-scale provider networks.
Forrester Report: 78% of US Enterprises Saw ROI Growth Using Managed Health Care
- Survey of Tier One enterprises indicates structured managed care improves cost efficiency, employee engagement, and overall ROI.
FAQ
Q1: What is the best managed health care plan for enterprises in the USA, UK, Canada, and Australia?
A: Hybrid HMO-PPO models with telehealth and wellness programs offer the best ROI and employee satisfaction.
Q2: How much does managed health care cost for businesses and organizations in Tier One markets?
A: Costs vary by coverage type, network size, and employee demographics, typically ranging from $400–$800 per employee monthly.
Q3: What are the top benefits of managed health care for ROI, lead generation, and conversions?
A: Cost containment, improved employee engagement, data-driven care decisions, and optimized provider networks.
Q4: Which managed care model (HMO, PPO, IPA) delivers the highest growth for employers?
A: Hybrid models combining HMO and PPO benefits deliver the highest ROI and growth potential.
Q5: How do enterprises compare managed health care plans for cost savings and ROI?
A: Through cost-benefit analysis, predictive analytics, provider performance evaluation, and employee feedback.
Q6: What is the ROI of investing in managed health care services for large employers?
A: ROI is realized via reduced healthcare costs, higher employee productivity, and enhanced retention rates.
Q7: What checklist should decision-makers follow before choosing a managed health care plan?
A: Evaluate network, costs, employee needs, data analytics capabilities, preventive care programs, and telehealth options.
Q8: What are the job and career opportunities in managed health care systems for professionals?
A: Roles include care coordinators, data analysts, policy advisors, and network managers.
Q9: Which managed health care providers offer the best services in the US, UK, Canada & Australia?
A: Top providers include UnitedHealthcare, Bupa, Medibank, and Sun Life Health Services.
Q10: How does managed health care improve patient outcomes, cost containment, and enterprise trust?
A: Through structured networks, preventive care, analytics-driven decision-making, and consistent quality standards.

